Advanced Analytics
Intake Efficiency
Our software includes masterful workflow, processes, information reporting, compliance checks and automation starting the process correctly to insure optimal submission and payment.
Collector Efficiency
Additional workflow, automation and reporting that leads to increased efficiency, productivity and collections for our clients. By identifying the % of claims that are denied after the invoices have been worked, we can train, correct issues and lower labor costs, resulting in lower rates for our clients!
Denials and Payment Trending Reporting
Our software and tools effectively model payer requirements, identify discrepancies for immediate correction pre-submission, decrease write offs by 50% or better and reduce lagging payments significantly.
Work History
Identifies trends and system updates by HCPCS, Item ID, payer and team members while quantifying issues, Eliminating the phrase “This happens a lot!”
Additional Benefits
Software Optimization
-Maintain price tables and fee schedules
-Review and implement enhancements
-Payer set up to include ERA

Clean Claim Rate
No manual intervention is needed, claim flows from confirmation to cash posting with no manual intervention

Data Analysis with recommendations for improvement
Monthly review of denial trending, invoice touches and payment activity
DSO by payer and payer group
ACU-Serve clients typically see AR over 90 less than 15%

Minimize write offs and adjustments
Data analysis to determine root causes
Share best practices and industry news
ACU-Serve is a member of AAHomecare, various state associations, and Medicare councils
ACU-Serve is powered by ACU-Insight
ACU-Insight, the engine that powers ACU-Serve, is a robust business analytics tool that allows providers to manage the revenue cycle with a holistic view. ACU-Serve developed the toolset to accommodate a client base with varied software platforms across numerous states and payers.
Work smarter not harder
ACU-Insight collects the data from multiple facets of your organization and delivers it in an actionable manner. By intelligently queuing up only the claims that need worked and eliminating unnecessary touches, ACU-Serve can reduce the number of claims being touched and in-turn lower the cost to its clients.
Improve profits through partnership
ACU-Insight empowers our clients to streamline processes and make changes that positively affect cash flow. By working smarter and continuously improving the way claims are managed from intake through cash posting, ACU-Serve strives to become a true Strategic Partner.
By partnering with ACU-Serve, providers are given the tools necessary to grow in today’s volatile market coupled with the expertise and best practices developed by ACU-Serve. These tools include:
- Customizable view tailored to the User
- Payer Trending
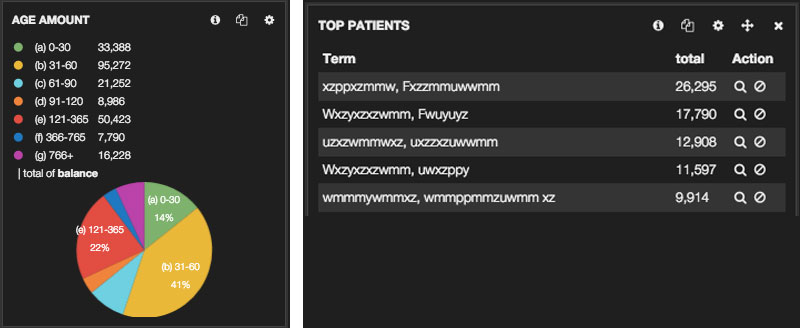
- Top Patient count and $$ amount
- Consistent feedback to help streamline intake processes
- Employee effectiveness tracking
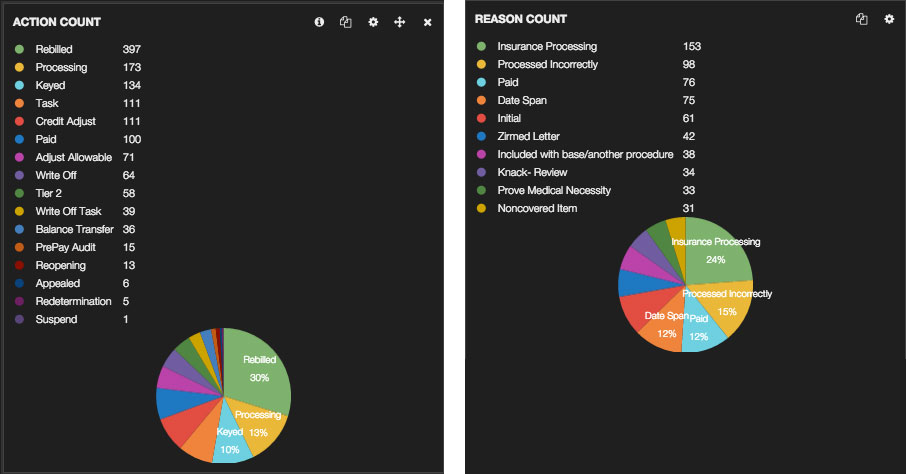
- Tracking and Trending of standardized Action and Reason codes
- Customizable AR reporting
- Invoice level reporting down to the Line Item/HCPC detail
- Easy change control tracking
- Data mining / Business analytics with limited impact on current business operations
ACU-Insight Workflow:
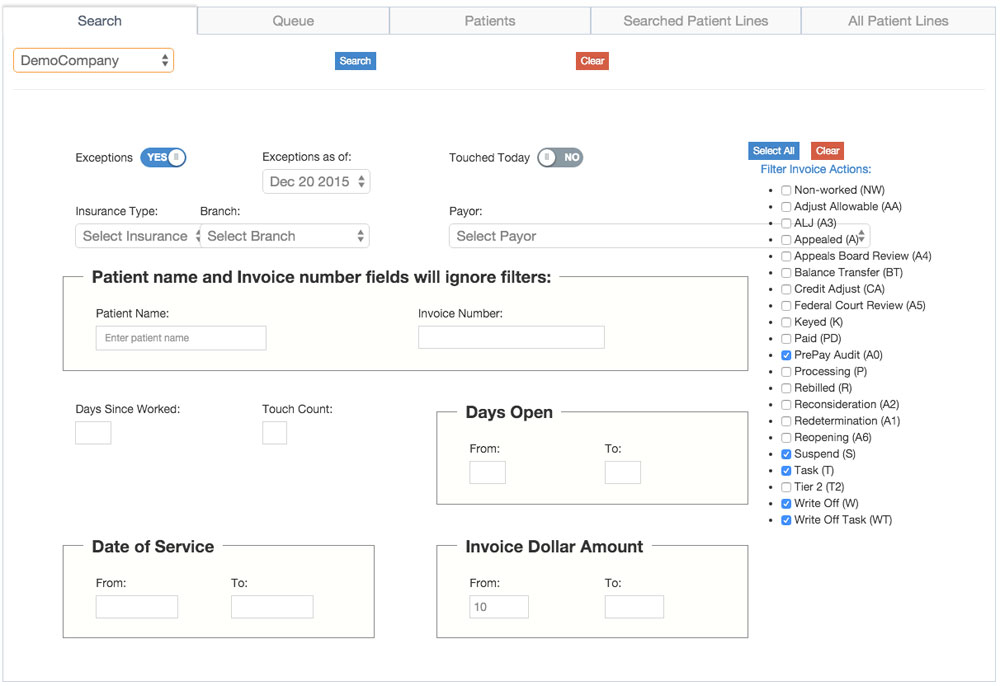
- Utilizes business intelligence to allow us to work smarter. Using average days to pay as a baseline for which invoices to work reduces wasted time and touches.
- Separate claims into work queues based on the product category to allow specialists with detailed knowledge to work the claims more effectively.
- Ability to note invoices with up to 3 levels of categorization: action taken, reason the action was taken and sub-reason in case more detail is needed.
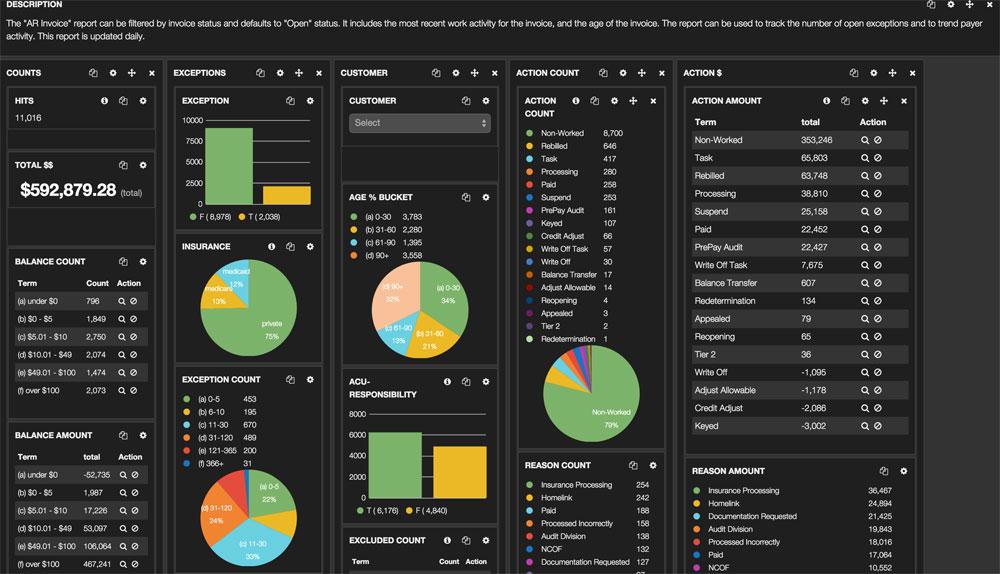
ACU-Insight Dashboard:
- Flexible, ad-hoc reporting capability with easy to read charts and graphs
-
Business analytics tool
- Provides insight into your business
- Provides transparency for how ACU-Serve is working for you
Common uses for ACU-Insight Dashboard
1. Where is my money?
a. Use the AR Invoice report to see aging information
b. You can click on each slice of the pie to get more detailed information about the invoices in each bucket. Why has my claim aged over 90 days? Is there a payer issue, a contract issue, a transmission issue, etc…?
c. Look at top patient balance to focus on high dollars claims
- a. Review the most common actions/reasons used over the last 30 days of work history.
- b. Drill into an action – click on Rebilled to get more information about which claims were rebilled and why. Identify price table, payer or other issues with your claims.